After sitting through several meetings last week, some of which included discussion of the value-based purchasing and readmission reduction programs that are included in the Affordable Care Act, I wonder how long it will take for the government (through Medicare-D plans) to implement similar programs that impact the world of community pharmacy.
You see, as pharmacy attempts to move forward and take a more proactive role in patient care we are going to be held accountable for results. Since individual pharmacists have not been granted provider status, the accountability will be passed to the actual pharmacy. This could be a good thing for the professional practice of pharmacy.
Now I have no knowledge of anything like what I am going to write about being in the works, but after hearing the presentation last week it seems entirely possible. And probably likely in the near future. Actually, I've wondered for quite a while about how long it would be until community pharmacies would be reimbursed based on performance. As the Affordable Care Act develops over the next several years, I can see similar programs being rolled out to the retail pharmacy.
Some of the measuring sticks for the hospital world under the value-based purchasing aspects of the ACA center on clinical outcomes, patient satisfaction scores, clinical outcomes, and efficiency in delivering medical care. This could very easily be translated to the community pharmacy setting. Can you imagine the change that would occur in the community pharmacy world if reimbursements were tied to things like time spent counseling patients, patient satisfaction scores, medication in-stock rates?
Imagine walking into a retail pharmacy and actually having a pharmacist be able to counsel a patient without worrying about falling behind by a dozen prescriptions. Imagine working at a pharmacy that has adequate pharmacist-staffing to allow for the patient interaction.
Of course this would have to be implemented in a manner similar to what is being done to hospitals. A certain percentage of reimbursements from government plans would be withheld, with pharmacies who achieve the goals receiving that money at the end of the year. This type of incentive would make some of the chain pharmacies focus less on the volume of prescriptions and more on the quality of care delivered to our patients.
Maybe extra reimbursements would be distributed to pharmacies that offer community education programs and show results. The few studies that have focused on the impact of pharmacist care on patient outcomes might actually be able to be implemented on a large scale.
What would happen if reimbursements were tied to the patient's perception of the care they receive at the pharmacy? If your patients believe that you are providing quality care and surveys back that up, you get an extra 4 or 5-percent on your reimbursements. I think the chains might react if better reimbursements are tied to the satisfaction scores.
The national pharmacy organizations have been pushing for inclusion of the pharmacist in the different health care models that are being debated. If we are included, we are going to need to show results. Be prepared to make the necessary changes and show your results.
Tuesday, October 23, 2012
Monday, October 8, 2012
Election day is on its way
I've found that as I get older, I have a greater appreciation for what the United States of America is. I have a tremendous amount of respect for the men and women who serve in our armed forces, preserving the freedoms that we have.
At the present time, I'm honored to have my children attend a school district where our veterans are honored. Our district has one of the top football programs in the state. The fans get jacked for our home games.
But at each home game, the crowd falls silent, rises to their feet, and honors our servicemen as an honor guard marches with the flag from one goal-line to the other. he crowd noise doesn't go down in volume a little bit. It is silent. You can hear a baby crying on the other side of the stadium. The amount of respect that is shown to our military by the crowd at the games is amazing. As soon as the honor guard comes to a halt, the band takes the field and the crowd gets back to its' pre-game craziness.
You don't see that in too many places anymore.
As we head into the election season, I encourage you to deliberate on what the United States of America is, and to vote for the candidates that represent the ideals of the United States.
One a side note... a local radio host has been playing this version of the Star-Spangled Banner over the airways quite a bit recently. After visiting the Smithsonian's American History museum a couple times over the last year or so and seeing the actual flag that the Star-Spangled Banner is written about, I have a greater appreciation for the words of the Star-Spangled Banner. Watch this video, reflect on the lyrics, and remember what the United States of America represents.
At the present time, I'm honored to have my children attend a school district where our veterans are honored. Our district has one of the top football programs in the state. The fans get jacked for our home games.
But at each home game, the crowd falls silent, rises to their feet, and honors our servicemen as an honor guard marches with the flag from one goal-line to the other. he crowd noise doesn't go down in volume a little bit. It is silent. You can hear a baby crying on the other side of the stadium. The amount of respect that is shown to our military by the crowd at the games is amazing. As soon as the honor guard comes to a halt, the band takes the field and the crowd gets back to its' pre-game craziness.
You don't see that in too many places anymore.
As we head into the election season, I encourage you to deliberate on what the United States of America is, and to vote for the candidates that represent the ideals of the United States.
One a side note... a local radio host has been playing this version of the Star-Spangled Banner over the airways quite a bit recently. After visiting the Smithsonian's American History museum a couple times over the last year or so and seeing the actual flag that the Star-Spangled Banner is written about, I have a greater appreciation for the words of the Star-Spangled Banner. Watch this video, reflect on the lyrics, and remember what the United States of America represents.
Wednesday, August 22, 2012
Free preventive care
Last night I received an email from the American Pharmacists Association that had a link to an article on the APhA website that caught my eye. This morning when I woke up, there were a few links to the same story on my Twitter timeline.
The story... Pharmacies team with HHS to promote free preventive care.
When I initially read the article on my smart phone, I read it as pharmacists providing care for free. That had my blood boiling and I wanted to jump all over the thought of free care. But I slept on it and re-read the article this morning.
The article states that there is growing recognition by HHS of the role that pharmacists play in a patient's health care. Personally I'm don't entirely agree with that, but I'll give that comment a pass.
HHS has, in what is called a pharmacist-friendly move, has partnered with pharmacists to.....
Drum roll
...
...
...
...
...
...
"...inform Medicare patients about free preventive services and the closing of the Part D coverage gap under the health care reform law."
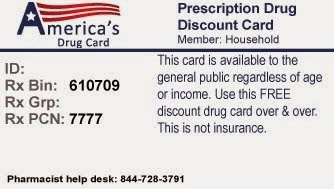
Pharmacists get to put up posters and pass out fliers on free preventive services for the Medicare population.
WOOHOO!!!
I was hoping to see pharmacists get the opportunity to provide services to the patients (and get reimbursed for said services). But this announcement is underwhelming to say the least.
C'mon APhA. Pharmacists need to be the providers. If we wanted to be the advertising department for HHS, we would have majored in advertising.
The story... Pharmacies team with HHS to promote free preventive care.
When I initially read the article on my smart phone, I read it as pharmacists providing care for free. That had my blood boiling and I wanted to jump all over the thought of free care. But I slept on it and re-read the article this morning.
The article states that there is growing recognition by HHS of the role that pharmacists play in a patient's health care. Personally I'm don't entirely agree with that, but I'll give that comment a pass.
HHS has, in what is called a pharmacist-friendly move, has partnered with pharmacists to.....
Drum roll
...
...
...
...
...
...
"...inform Medicare patients about free preventive services and the closing of the Part D coverage gap under the health care reform law."
Pharmacists get to put up posters and pass out fliers on free preventive services for the Medicare population.
WOOHOO!!!
I was hoping to see pharmacists get the opportunity to provide services to the patients (and get reimbursed for said services). But this announcement is underwhelming to say the least.
C'mon APhA. Pharmacists need to be the providers. If we wanted to be the advertising department for HHS, we would have majored in advertising.
Tuesday, August 14, 2012
Should I become a pharmacist?
One of my oldest son's friends is entering her senior year of high school this year. Her plans after graduation...attend pharmacy school in order to become the clinical pharmacist in a children's hospital. An admirable career choice.
But, in my opinion, she's about ten years late on entering the pharmacy profession. I've told my son that I need to have a conversation with her before she totally commits to the profession.
Do I believe that she can make it through the academics? Absolutely. She has been taking advanced courses at the local college instead of regular high school classes since the start of her junior year.
The problem lies in the fact that about eighty-seven kajillion pharmacy programs have opened up in the last decade. Remember the days when pharmacists were in demand? Those days have long passed us. We are now facing a flooded jobs market.
With a typical course of study running eight years and debt loads pushing the quarter-million dollar mark, is it advisable to enter a profession where there are no guaranteed jobs? For basically the same amount of schooling you can become a physician. When I look at the news stories and see that there is going to be a shortage of physicians, I am inclined to believe that medicine is a better career path. Heck, I still toy with the idea of leaving pharmacy to go back to medical school.
Now pharmacy is still an excellent career, especially if your employer treats you with the respect that should be afforded to somebody with an advanced degree. But too many of our colleagues are still being treated as merely a name on a license that can easily be replaced if they so much as voice concerns about the working conditions.
In my previous position, due to sales and script volume not reaching budgeted amounts, I was shipped out to neighboring pharmacies in my chain to work a few shifts each month. After a shift where I personally checked over 475 scripts in a 10 hour shift, I decided that it was time to leave that particular company. I was fortunate enough to have a physician friend tell me about an open director of pharmacy position at a local critical access hospital. A couple interviews later I was on my way out of retail pharmacy. I was lucky.
Not everybody has connections that can lead to the better jobs, especially new graduates in a flooded market. Even a resume with a residency doesn't guarantee a position.
I put the blame for the flooded market on both academia and the big chains. The prospects of four years of extra tuition has the financial folks at the universities going gaga over the thoughts of opening up their own programs. Especially when they can quote a six-figure salary upon completion of the program. To any person checking out a pharmacy school, be sure to find out what percentage of their graduates have jobs upon graduation and three months after graduation. I'm fairly certain it won't be in the high 90s like it was when I graduated in the mid 1990s.
Then there's the influence of the chains. They will tell you that they wanted more pharmacists due to the shortage that we saw in the mid-to-late 90s. I can buy that to some extent, but my conspiracy-driven brain thinks that they were actually looking at the staffing issues from a supply-and-demand aspect. If they could get the supply of pharmacists to exceed the demand, then they could start to drive down salaries and benefits, and thus increase their bottom line. Don't believe me? Check out some of the proposed concessions that Dave Stanley wrote about in a recent Drug Topics article. A major employer was wanting to shift the costs of benefits over to the pharmacists, while cutting the hours that the pharmacists were able to work each week.
If I'm entering the job market right now (or actually four to eight years from now), that's not what I would want to be facing. I'm hopeful that the job market will correct itself, but if I were to offer advice right now I'd tell you to look at another option in the medical professions.
But, in my opinion, she's about ten years late on entering the pharmacy profession. I've told my son that I need to have a conversation with her before she totally commits to the profession.
Do I believe that she can make it through the academics? Absolutely. She has been taking advanced courses at the local college instead of regular high school classes since the start of her junior year.
The problem lies in the fact that about eighty-seven kajillion pharmacy programs have opened up in the last decade. Remember the days when pharmacists were in demand? Those days have long passed us. We are now facing a flooded jobs market.
With a typical course of study running eight years and debt loads pushing the quarter-million dollar mark, is it advisable to enter a profession where there are no guaranteed jobs? For basically the same amount of schooling you can become a physician. When I look at the news stories and see that there is going to be a shortage of physicians, I am inclined to believe that medicine is a better career path. Heck, I still toy with the idea of leaving pharmacy to go back to medical school.
Now pharmacy is still an excellent career, especially if your employer treats you with the respect that should be afforded to somebody with an advanced degree. But too many of our colleagues are still being treated as merely a name on a license that can easily be replaced if they so much as voice concerns about the working conditions.
In my previous position, due to sales and script volume not reaching budgeted amounts, I was shipped out to neighboring pharmacies in my chain to work a few shifts each month. After a shift where I personally checked over 475 scripts in a 10 hour shift, I decided that it was time to leave that particular company. I was fortunate enough to have a physician friend tell me about an open director of pharmacy position at a local critical access hospital. A couple interviews later I was on my way out of retail pharmacy. I was lucky.
Not everybody has connections that can lead to the better jobs, especially new graduates in a flooded market. Even a resume with a residency doesn't guarantee a position.
I put the blame for the flooded market on both academia and the big chains. The prospects of four years of extra tuition has the financial folks at the universities going gaga over the thoughts of opening up their own programs. Especially when they can quote a six-figure salary upon completion of the program. To any person checking out a pharmacy school, be sure to find out what percentage of their graduates have jobs upon graduation and three months after graduation. I'm fairly certain it won't be in the high 90s like it was when I graduated in the mid 1990s.
Then there's the influence of the chains. They will tell you that they wanted more pharmacists due to the shortage that we saw in the mid-to-late 90s. I can buy that to some extent, but my conspiracy-driven brain thinks that they were actually looking at the staffing issues from a supply-and-demand aspect. If they could get the supply of pharmacists to exceed the demand, then they could start to drive down salaries and benefits, and thus increase their bottom line. Don't believe me? Check out some of the proposed concessions that Dave Stanley wrote about in a recent Drug Topics article. A major employer was wanting to shift the costs of benefits over to the pharmacists, while cutting the hours that the pharmacists were able to work each week.
If I'm entering the job market right now (or actually four to eight years from now), that's not what I would want to be facing. I'm hopeful that the job market will correct itself, but if I were to offer advice right now I'd tell you to look at another option in the medical professions.
Tuesday, July 10, 2012
Pharmacist prescribing
It hardy seems like it, but Monday was the one year anniversary of my switch from retail/community pharmacy to the hospital setting. After 16 years behind the counter I have spent the last twelve months behind a desk and have loved every minute of it.
Over this past year, I've been able to see the successes in the health care industry. I've also seen some of the failures of the system. Some of my more memorable moments have come when I have been able to work with our interdisciplinary team and contribute to positive patient outcomes. I feel that I have earned the respect of the hospitalists and the nursing staff on our main patient floor.
One of the key things that I've found that has helped me earn their respect is to ask how the pharmacy service can help make their lives easier. There have been instances where I have made their lives more difficult as well. When that has happened, it didn't take long for somebody to explain the situation to me and I made the adjustments to correct the situation. The key to this has been open communication and open minds.
Open communication.....
Hmmmmm.......
Over the past year I haven't seen a whole lot of news in the pharmacy world. The only three "big" stories that I can think of are the Express Scripts-Medco merger, the move for more OTC/behind-the-counter medications, and pharmacists gaining prescriptive authority.
When I read articles/blogs/tweets on the prescribing issue, I keep seeing the same things. Pharmacists are the medication experts, so why shouldn't we be able to prescribe. I have my personal opinion on the issue, but I would like to ask a question that I haven't seen addressed anywhere.
Have we asked if the other members of the health care team want us to have have prescriptive authority? Do the physicians want us to have that authority? Has anybody in pharmacy actually communicated with the AMA and asked them for their thoughts on how the pharmacy profession can help the doctors?
It seems to me that pharmacist prescribing may be another idea dreamed up in academia that might not be able to fly in the real world. I've seen links to several stories lately that shows that the medical doctors really don't want us to prescribe.
Does anybody know if this has been addressed with our medical colleagues? If so, please share.
Over this past year, I've been able to see the successes in the health care industry. I've also seen some of the failures of the system. Some of my more memorable moments have come when I have been able to work with our interdisciplinary team and contribute to positive patient outcomes. I feel that I have earned the respect of the hospitalists and the nursing staff on our main patient floor.
One of the key things that I've found that has helped me earn their respect is to ask how the pharmacy service can help make their lives easier. There have been instances where I have made their lives more difficult as well. When that has happened, it didn't take long for somebody to explain the situation to me and I made the adjustments to correct the situation. The key to this has been open communication and open minds.
Open communication.....
Hmmmmm.......
Over the past year I haven't seen a whole lot of news in the pharmacy world. The only three "big" stories that I can think of are the Express Scripts-Medco merger, the move for more OTC/behind-the-counter medications, and pharmacists gaining prescriptive authority.
When I read articles/blogs/tweets on the prescribing issue, I keep seeing the same things. Pharmacists are the medication experts, so why shouldn't we be able to prescribe. I have my personal opinion on the issue, but I would like to ask a question that I haven't seen addressed anywhere.
Have we asked if the other members of the health care team want us to have have prescriptive authority? Do the physicians want us to have that authority? Has anybody in pharmacy actually communicated with the AMA and asked them for their thoughts on how the pharmacy profession can help the doctors?
It seems to me that pharmacist prescribing may be another idea dreamed up in academia that might not be able to fly in the real world. I've seen links to several stories lately that shows that the medical doctors really don't want us to prescribe.
Does anybody know if this has been addressed with our medical colleagues? If so, please share.
Wednesday, March 21, 2012
Who benefits from more OTC medications?
Thursday and Friday (March 22 & 23) the FDA is holding its public hearings on "using innovative technologies and other conditions of safe use to expand drug products considered nonprescription". You know, moving more drug categories to OTC status.
The initial response that I had, and that has been voiced through several outlets, is that this may be the step that is needed to enable pharmacists to be recognized as providers. My thoughts were that this should not move forward unless the OTC move was restricted to pharmacies-only with a built-in means for reimbursement to the pharmacists providing the consultation. This would keep the consultation separate from the drug product. This could be very good for the profession.
But now I've had a few days to mull this around in my head. Something just doesn't sit well with me on this.
I've never known our government or any of its agencies to move quickly on issues, especially when it comes to our profession. But for this issue, the notification for the hearing was filed on February 27, published in the Federal Register on February 28, with a deadline to present oral comments & presentations of March 9. That's less than two weeks. With the hearing being held less than two weeks after the deadline.
3-1/2 weeks from the notice of hearing in the Federal Register until the hearings begin seems to be moving rather quick to me. Which makes me skeptical.
Who are the entities that are pushing for this?
Who has been working behind the scenes with the FDA to get this agenda advanced? How much have they prepared for the hearings prior to the announcement?
It will be interesting to see who actually makes oral presentations and comments at the hearings. With such short notice, I doubt that there will be very many, if any, practicing pharmacists at the hearings.
My concern is that the entities who stand to profit the most from this will dominate the hearings and the voice of the practicing pharmacists will not be heard. And we all know who stands to profit the most.
Manufacturers.
Insurers.
Chains.
Manufacturers know that moving the items from prescription status to non-prescription status will decrease the competition for their product. Not too many manufacturers are competing for the generic OTC market, so the brand-name manufacturers can keep a better market share by going OTC. When you consider the rebates that they must give on Medicare/Medicaid scripts, they potentially will make more profit with the switch.
Then there are the insurers. No-brainer for them. Our plan does not cover over-the-counter medications. They can eliminate several medications that are standard on formularies. For them, OTC = $$$.
Then there are the chain pharmacies. We all know that the chains are looking to decrease labor costs, especially pharmacist labor. Sure the move of certain medications to OTC status will decrease script counts, but that gives them a reason to decrease pharmacist payroll. Nevermind that the pharmacist will get pulled aside every seven minutes to consult a patient about these new OTC meds. Chain pharmacy staffing follows a simple equation... X scripts/hr/pharmacist. If you are not hitting the numbers, you lose the payroll. The profit on an OTC medication is better than the standard dispensing fee from insurers, so why wouldn't the chains be on-board?
I hope my gut is wrong on this one. But less than four weeks from the time of announcement until the FDA hearing just makes me think that something funny is going on... and not for the betterment of our profession.
What do you think?
The initial response that I had, and that has been voiced through several outlets, is that this may be the step that is needed to enable pharmacists to be recognized as providers. My thoughts were that this should not move forward unless the OTC move was restricted to pharmacies-only with a built-in means for reimbursement to the pharmacists providing the consultation. This would keep the consultation separate from the drug product. This could be very good for the profession.
But now I've had a few days to mull this around in my head. Something just doesn't sit well with me on this.
I've never known our government or any of its agencies to move quickly on issues, especially when it comes to our profession. But for this issue, the notification for the hearing was filed on February 27, published in the Federal Register on February 28, with a deadline to present oral comments & presentations of March 9. That's less than two weeks. With the hearing being held less than two weeks after the deadline.
3-1/2 weeks from the notice of hearing in the Federal Register until the hearings begin seems to be moving rather quick to me. Which makes me skeptical.
Who are the entities that are pushing for this?
Who has been working behind the scenes with the FDA to get this agenda advanced? How much have they prepared for the hearings prior to the announcement?
It will be interesting to see who actually makes oral presentations and comments at the hearings. With such short notice, I doubt that there will be very many, if any, practicing pharmacists at the hearings.
My concern is that the entities who stand to profit the most from this will dominate the hearings and the voice of the practicing pharmacists will not be heard. And we all know who stands to profit the most.
Manufacturers.
Insurers.
Chains.
Manufacturers know that moving the items from prescription status to non-prescription status will decrease the competition for their product. Not too many manufacturers are competing for the generic OTC market, so the brand-name manufacturers can keep a better market share by going OTC. When you consider the rebates that they must give on Medicare/Medicaid scripts, they potentially will make more profit with the switch.
Then there are the insurers. No-brainer for them. Our plan does not cover over-the-counter medications. They can eliminate several medications that are standard on formularies. For them, OTC = $$$.
Then there are the chain pharmacies. We all know that the chains are looking to decrease labor costs, especially pharmacist labor. Sure the move of certain medications to OTC status will decrease script counts, but that gives them a reason to decrease pharmacist payroll. Nevermind that the pharmacist will get pulled aside every seven minutes to consult a patient about these new OTC meds. Chain pharmacy staffing follows a simple equation... X scripts/hr/pharmacist. If you are not hitting the numbers, you lose the payroll. The profit on an OTC medication is better than the standard dispensing fee from insurers, so why wouldn't the chains be on-board?
I hope my gut is wrong on this one. But less than four weeks from the time of announcement until the FDA hearing just makes me think that something funny is going on... and not for the betterment of our profession.
What do you think?
Thursday, March 15, 2012
But you didn't.......
Today starts the beginning of the NCAA Basketball tournament. St.Patrick's Day and all of its merriment is a couple days away.
I came upon this a couple days ago on one of the apps that I waste time on. I don't know if it was written by somebody who actually suffered a loss, but this struck a chord with me.
As we go about celebrating springtime here in the United States let us remember those who aren't safe at home, but are allowing us to be safe at home.

I came upon this a couple days ago on one of the apps that I waste time on. I don't know if it was written by somebody who actually suffered a loss, but this struck a chord with me.
As we go about celebrating springtime here in the United States let us remember those who aren't safe at home, but are allowing us to be safe at home.

Monday, March 12, 2012
Medications available under "safe use"
Recently I came upon a blog post by APhA CEO Tom Menighan where he brings up the FDA's idea of making certain prescription medications available without a prescription, provided that the medications are provided under conditions of safe use.
This proposal combines a couple of the ideas that have been floating around for several years...a pharmacist-only class of medications as well as limited pharmacist prescribing. Under one safe use provisions, the sale of these agents might be limited to certain health care settings, such as a pharmacy. I emphasize the word might, as Docket No. FDA-2012-N-0171 use the word might rather than would when it discusses whether or not the sales would be restricted to pharmacies.
I believe that this proposal is a step in the right direction for pharmacy. Opening up access to pharmacists as providers with limited prescriptive authority could ease the burden on primary care practitioners and help advance our profession. My concern is that pharmacy will provide this service without ensuring a reimbursement structure for the pharmacists who are providing the service.
We can't continue to give away our services without getting paid because face it, at the end of the day pharmacy is still a business and if your business isn't generating cash-flow it won't be a business very long. This may be the chance that our profession can capitalize on and be granted the provider status that we have been petitioning for over the last several years.
We need to make sure that the regulations contain language that requires pharmacist intervention, not suggests or recommends t. We also need to make sure that provisions are included that allow for reimbursement for services. We can't rely on building the professional fee into the price of the product because people will not see our services as being professional. They will simply look for the pharmacy that has the lowest price and go there. The consultation with the pharmacist must be removed from the product if we truly hope to advance the professional scope of our practice.
Sorry for getting this out so late. The notice came out in the Federal Register on Feb 28 and the deadline for being able to present oral presentations and comments has already passed. However, electronic and written comments will be accepted until May 7, 2012. I encourage you to chime in on this topic.
This proposal combines a couple of the ideas that have been floating around for several years...a pharmacist-only class of medications as well as limited pharmacist prescribing. Under one safe use provisions, the sale of these agents might be limited to certain health care settings, such as a pharmacy. I emphasize the word might, as Docket No. FDA-2012-N-0171 use the word might rather than would when it discusses whether or not the sales would be restricted to pharmacies.
I believe that this proposal is a step in the right direction for pharmacy. Opening up access to pharmacists as providers with limited prescriptive authority could ease the burden on primary care practitioners and help advance our profession. My concern is that pharmacy will provide this service without ensuring a reimbursement structure for the pharmacists who are providing the service.
We can't continue to give away our services without getting paid because face it, at the end of the day pharmacy is still a business and if your business isn't generating cash-flow it won't be a business very long. This may be the chance that our profession can capitalize on and be granted the provider status that we have been petitioning for over the last several years.
We need to make sure that the regulations contain language that requires pharmacist intervention, not suggests or recommends t. We also need to make sure that provisions are included that allow for reimbursement for services. We can't rely on building the professional fee into the price of the product because people will not see our services as being professional. They will simply look for the pharmacy that has the lowest price and go there. The consultation with the pharmacist must be removed from the product if we truly hope to advance the professional scope of our practice.
Sorry for getting this out so late. The notice came out in the Federal Register on Feb 28 and the deadline for being able to present oral presentations and comments has already passed. However, electronic and written comments will be accepted until May 7, 2012. I encourage you to chime in on this topic.
Monday, January 23, 2012
Something to chew on
I logged on to Facebook the other day and saw a status update from one of the guys from my high school days. He was commenting on the service that he received from a few different pharmacies as he was attempting to find on of the medications that is currently in short-supply.
Would it surprise you to find out that one of the national chains didn't even acknowledge him standing at the drop-off window? Not a "we'll be with you in a moment". Not a nod from a pharmacist or tech to let him know that they spotted him. In fact, two different techs/cashiers walked past him at the drop-off window on their way to the pick-up window to wait on people who entered the pharmacy after he did.
Once he was finally waited on, it took over thirty minutes for the pharmacy staff to inform him that the medication was not available. Needless to say, he was disappointed with the service that he received at the pharmacy. Not one to remain quiet, he addressed the store manager about the "extra care" that he received. Did he receive an "I'm sorry" or any form of compassion from the manager?
Nope.
The manager pointed to a customer comments phone number that was posted on a sign and was told to call the number.
He went to another pharmacy and was able to obtain the medication. In and out, with pharmacist consultation, in under 15 minutes. He was singing praises about the pharmacy that took care of him. Even to the point of giving the address of the pharmacy in the comments after his post.
In my retail days, I never really thought about how people would comment about the care that they received at my pharmacy on the social media sites. We hear about word-of-mouth advertising, but this was the first time that I have seen it play out in the social media. The volume of comments that his update generated was astounding.
If we, as pharmacists, want to be recognized as individual medical providers then the type of service that the first pharmacy provided is unacceptable. Patients aren't going to want to see providers who ignore their presence for 15 minutes. Sadly, this type of service is common from what I've seen of the first pharmacy chain.
If we want to advance the scope of our practice, we need to provide care that exceeds the patient's expectations. We want the social media to have complements about our profession, not complaints.
Isn't there a saying that says it takes 10 positive comments to cancel the effects of one negative one. Maybe we should set that as our benchmark for how we see pharmacy experiences reported in the social media.
Just something to chew on for a little bit.
Would it surprise you to find out that one of the national chains didn't even acknowledge him standing at the drop-off window? Not a "we'll be with you in a moment". Not a nod from a pharmacist or tech to let him know that they spotted him. In fact, two different techs/cashiers walked past him at the drop-off window on their way to the pick-up window to wait on people who entered the pharmacy after he did.
Once he was finally waited on, it took over thirty minutes for the pharmacy staff to inform him that the medication was not available. Needless to say, he was disappointed with the service that he received at the pharmacy. Not one to remain quiet, he addressed the store manager about the "extra care" that he received. Did he receive an "I'm sorry" or any form of compassion from the manager?
Nope.
The manager pointed to a customer comments phone number that was posted on a sign and was told to call the number.
He went to another pharmacy and was able to obtain the medication. In and out, with pharmacist consultation, in under 15 minutes. He was singing praises about the pharmacy that took care of him. Even to the point of giving the address of the pharmacy in the comments after his post.
In my retail days, I never really thought about how people would comment about the care that they received at my pharmacy on the social media sites. We hear about word-of-mouth advertising, but this was the first time that I have seen it play out in the social media. The volume of comments that his update generated was astounding.
If we, as pharmacists, want to be recognized as individual medical providers then the type of service that the first pharmacy provided is unacceptable. Patients aren't going to want to see providers who ignore their presence for 15 minutes. Sadly, this type of service is common from what I've seen of the first pharmacy chain.
If we want to advance the scope of our practice, we need to provide care that exceeds the patient's expectations. We want the social media to have complements about our profession, not complaints.
Isn't there a saying that says it takes 10 positive comments to cancel the effects of one negative one. Maybe we should set that as our benchmark for how we see pharmacy experiences reported in the social media.
Just something to chew on for a little bit.
AMA vs APhA.... looking out for the interests of their members
Just a quick note on this article that I found on Twitter today.
The AMA pays close attention to the reimbursements that its members receive from third-parties and addresses the issues instantly. Whenever the evening news announces a cut in Medicare reimbursement rates, you can put money down that the AMA will have a statement releases by the start of the next day's news cycle. The AMA understands that without adequate reimbursement, the standard of care will drop and businesses will fail. In the article that I link to, the AMA offers ideas for its members who might be a little cash-strapped.
Let's compare that to the APhA.
The big topics in retail pharmacy over the last couple months has been the Walgreens-Express Scripts drama over reimbursements.
I did a little search on the APhA website to see if there was any commentary on the issue. From the home page I searched for "Express Scripts". Top search result...a 2007 article about drug prices.
So I went over to the APhA CEO blog. With the edit button of my browser I did a "Ctrl+F" (Find on this page) search for "express". Only one match for "express" among the ten blog posts. You probably already know that it didn't match up to Express Scripts.
One of the biggest stories in pharmacy, centering around reimbursement issues, and the APhA has yet to address the issues on its web-site.
Rule #1 for business. You must make money to stay in business. The AMA gets it.
The AMA pays close attention to the reimbursements that its members receive from third-parties and addresses the issues instantly. Whenever the evening news announces a cut in Medicare reimbursement rates, you can put money down that the AMA will have a statement releases by the start of the next day's news cycle. The AMA understands that without adequate reimbursement, the standard of care will drop and businesses will fail. In the article that I link to, the AMA offers ideas for its members who might be a little cash-strapped.
Let's compare that to the APhA.
The big topics in retail pharmacy over the last couple months has been the Walgreens-Express Scripts drama over reimbursements.
I did a little search on the APhA website to see if there was any commentary on the issue. From the home page I searched for "Express Scripts". Top search result...a 2007 article about drug prices.
So I went over to the APhA CEO blog. With the edit button of my browser I did a "Ctrl+F" (Find on this page) search for "express". Only one match for "express" among the ten blog posts. You probably already know that it didn't match up to Express Scripts.
One of the biggest stories in pharmacy, centering around reimbursement issues, and the APhA has yet to address the issues on its web-site.
Rule #1 for business. You must make money to stay in business. The AMA gets it.
Tuesday, January 10, 2012
Pharmacists as providers?
This past weekend marked the six-month anniversary of my transition from retail to hospital pharmacy. It seems like only yesterday that I was behind the pharmacy counter, while it also seems like forever since I’ve been in a community pharmacy.
One thing that immediately jumps out at me on the difference between the two settings is the manner in which I am treated as a pharmacist. In the retail setting, physicians and nurses (or receptionists or whoever the physician allows to represent them on the phone) didn’t seem to respect the knowledge of the pharmacist. I felt that I was viewed as a nuisance. Not so in the hospital setting. On a daily basis I am asked for my input on decisions relating to the care of my patients. A vast majority of the time my recommendations are accepted and implemented.
It didn’t take long for me to realize that hospital and community pharmacy are worlds apart with regards to the practice of pharmacy. I follow what is happening in the retail sector through blog posts and Twitter updates, but for the most part the issues in retail have no bearing on my practice in the hospital setting. And by the same token the issues that hospital pharmacists face don’t mean a whole lot to the folks out in the retail trenches.
The profession is clearly divided and it’s no surprise that pharmacy isn’t represented that well by the national organizations. There isn’t an issue that all of us can get on board with in order to have a united voice. So you end up having several different organizations (NCPA, ASHP, ASCP, etc…) representing their individual interests, trying to talk over each other and in the end nobody’s voice is heard.
The American Pharmacist Association, in my opinion, should be the organization that should be able to speak for all pharmacists. If you pay attention to the opinions expressed on the social media, pharmacists don’t feel that the APhA is doing much, if anything, to address the issues that pharmacists are facing.
The APhA has totally bought-in to the medication therapy management (MTM) practice model. Over the past 18 to 24 months, various articles have tried to sell MTM as the pharmacist’s component of accountable care organizations, patient-centered medical homes, and collaborative practice arrangements. While I believe that MTM-style services are where pharmacy should be heading, I believe that the so-called leaders of the profession missed a key component of the equation when they decided to go all-in on MTM.
Reimbursement.
Sure, some Medicare Part D plans are reimbursing pharmacists for MTM services, such as comprehensive medication reviews. But these are limited to the patients who are selected by the insurers. Rather than accept the practice model no-questions-asked, how about taking a step back to get all of our ducks in a row? How about getting us recognized as providers so that MTM services are reimbursable from all insurers and can be offered to all patients instead of the select few Medicare Part D-ers.
The first issue that should have been addressed is recognition of pharmacists as medical providers. If pharmacists receive provider status and are able to bill for services rendered, the entire MTM practice model will take off. There are innovative minds in the pharmacy world that will revolutionize healthcare, but we need to be sure that the bills will be paid at the end of the day. Changing the practice model today with the hopes of reimbursement tomorrow isn’t going to cut it. We need to become recognized providers now. There is a petition floating around out there to try to get pharmacists recognized as providers. If you haven’t done so already, I suggest that you check it out.
Provider status is the issue that covers a majority of the practice settings for pharmacists and could unite the profession into a strong voice. Over a year ago I wrote on how different practice settings could benefit from being recognized as providers*. Community pharmacists could bill professional fees for DURs, OTC consults, and even calls to insurers (nowhere in my state’s pharmacy practice act does it state that pharmacists must call insurance companies). For each service that we provide, we should bill. The days of counting on dispensing fees to cover the costs of these services are long gone. Pharmacists need to be reimbursed for the professional services that are provided.
On the hospital and consultant side, pharmacists could charge for consults and interventions that occur daily. These are documented at many facilities; we just need to develop a charge sheet to be able to submit to the insurers and Medicare. Services such as anticoagulation clinics, diabetes/asthma/COPD-education, and nutrition education would be areas where pharmacists could make a huge difference if the reimbursements were there.
I don’t know what it’s going to take for pharmacists to unite as one voice. It might be the APhA taking the lead and pushing for recognition as providers. It could be retail pharmacists saying enough is enough and forming a union to get issues addressed.
Whatever the practice setting, I think that we all can agree that we need to be paid fairly for what we do as professionals. Recognition as providers is the first step towards achieving that goal.
*Previous posts of mine that address this issue
One thing that immediately jumps out at me on the difference between the two settings is the manner in which I am treated as a pharmacist. In the retail setting, physicians and nurses (or receptionists or whoever the physician allows to represent them on the phone) didn’t seem to respect the knowledge of the pharmacist. I felt that I was viewed as a nuisance. Not so in the hospital setting. On a daily basis I am asked for my input on decisions relating to the care of my patients. A vast majority of the time my recommendations are accepted and implemented.
It didn’t take long for me to realize that hospital and community pharmacy are worlds apart with regards to the practice of pharmacy. I follow what is happening in the retail sector through blog posts and Twitter updates, but for the most part the issues in retail have no bearing on my practice in the hospital setting. And by the same token the issues that hospital pharmacists face don’t mean a whole lot to the folks out in the retail trenches.
The profession is clearly divided and it’s no surprise that pharmacy isn’t represented that well by the national organizations. There isn’t an issue that all of us can get on board with in order to have a united voice. So you end up having several different organizations (NCPA, ASHP, ASCP, etc…) representing their individual interests, trying to talk over each other and in the end nobody’s voice is heard.
The American Pharmacist Association, in my opinion, should be the organization that should be able to speak for all pharmacists. If you pay attention to the opinions expressed on the social media, pharmacists don’t feel that the APhA is doing much, if anything, to address the issues that pharmacists are facing.
The APhA has totally bought-in to the medication therapy management (MTM) practice model. Over the past 18 to 24 months, various articles have tried to sell MTM as the pharmacist’s component of accountable care organizations, patient-centered medical homes, and collaborative practice arrangements. While I believe that MTM-style services are where pharmacy should be heading, I believe that the so-called leaders of the profession missed a key component of the equation when they decided to go all-in on MTM.
Reimbursement.
Sure, some Medicare Part D plans are reimbursing pharmacists for MTM services, such as comprehensive medication reviews. But these are limited to the patients who are selected by the insurers. Rather than accept the practice model no-questions-asked, how about taking a step back to get all of our ducks in a row? How about getting us recognized as providers so that MTM services are reimbursable from all insurers and can be offered to all patients instead of the select few Medicare Part D-ers.
The first issue that should have been addressed is recognition of pharmacists as medical providers. If pharmacists receive provider status and are able to bill for services rendered, the entire MTM practice model will take off. There are innovative minds in the pharmacy world that will revolutionize healthcare, but we need to be sure that the bills will be paid at the end of the day. Changing the practice model today with the hopes of reimbursement tomorrow isn’t going to cut it. We need to become recognized providers now. There is a petition floating around out there to try to get pharmacists recognized as providers. If you haven’t done so already, I suggest that you check it out.
Provider status is the issue that covers a majority of the practice settings for pharmacists and could unite the profession into a strong voice. Over a year ago I wrote on how different practice settings could benefit from being recognized as providers*. Community pharmacists could bill professional fees for DURs, OTC consults, and even calls to insurers (nowhere in my state’s pharmacy practice act does it state that pharmacists must call insurance companies). For each service that we provide, we should bill. The days of counting on dispensing fees to cover the costs of these services are long gone. Pharmacists need to be reimbursed for the professional services that are provided.
On the hospital and consultant side, pharmacists could charge for consults and interventions that occur daily. These are documented at many facilities; we just need to develop a charge sheet to be able to submit to the insurers and Medicare. Services such as anticoagulation clinics, diabetes/asthma/COPD-education, and nutrition education would be areas where pharmacists could make a huge difference if the reimbursements were there.
I don’t know what it’s going to take for pharmacists to unite as one voice. It might be the APhA taking the lead and pushing for recognition as providers. It could be retail pharmacists saying enough is enough and forming a union to get issues addressed.
Whatever the practice setting, I think that we all can agree that we need to be paid fairly for what we do as professionals. Recognition as providers is the first step towards achieving that goal.
*Previous posts of mine that address this issue
- State of the Profession.....Unity
State of the Profession, Part Two...Organization
State of the Profession.... Reimbursement Part I
State of the profession.....Reimbursements Part II
A change in thinking
CTP codes. How about CPS codes?
Pharmacist reimbursement for professional aspects of dispensing
Reimbursement for OTC consults
Subscribe to:
Posts (Atom)