Thursday, February 24, 2011
Thoughts on health care reform
It was a prescription for an oral contraceptive. I explained that the pharmacy benefits manager might cover the medication if the prescriber submits documentation that the medication is being used for something other than the prevention of pregnancy.
But isn't it less expensive for them to cover the birth control pills instead of the cost of a pregnancy and delivery?
Well, you think that the answer would be yes. But your medical insurance company and your pharmacy benefits manager are two different companies. The company that handles your prescription coverage has no vested interest in keeping you from becoming pregnant. They don't handle your hospital bills. Why should they worry about it? Their only job is to keep medication costs down.
That was a conversation I had with one of my patients a few weeks ago. And it's a conversation I'll have dozens more times over the remainder of this year. And next year. And the year after that.
With the passage of the Affordable Care Act and the recent court ruling that held parts of the act to be unconstitutional, we have no idea where health care reform is going. But I think we can all agree that something is going to be done. It's just that none of us know what that will be.
I don't have the answers on health care reform, but I wanted to share a few of my thoughts on the issue.
In my opinion, one of the largest obstacles to care is the segmentation that occurs between the different companies that insure the patients. One company covers visits to the physician and hospital, another company covers dental health, and a third company covers the prescription medications. There may even be another company that handles vision care. There is no coordination of care since the insurers are separate companies. Each company is primarily interested in minimizing their costs. Patient care may not always be at the forefront of each company's thought processes.
Rather than continuing down the road we are on, I think that insurers should cover all aspects of patient care. Not just one segment of it.
Patients would have one company looking out for their total health care. Medical, dental, vision, and prescription coverage all from the same company. Then maybe little Johnny won't need to try three different medications before his Singulair is covered to control his asthma and allergies because the insurer knows that little Johnny will most likely have three ER visits in the meantime and run up enormous bills that could be avoided simply by covering the medication in the first place.
At the same time, the insurer would be able to track patient compliance because they would have all of the patient records at their hands. Let's say Mr Smith is diagnosed with asthma by his physician. The physician orders a steroid inhaler and a rescue inhaler. This information is transmitted to the insurer when the physician submits their bill. The insurer is able to see if Mr Smith is filling his prescriptions for both medications on a regular basis.
If Mr Smith runs to the ER with difficulty breathing and hasn't filled his prescription for the steroid in a while, the insurer can contact the prescriber and the issue can be addressed. If the patient continues to not fill his prescriptions and keeps running to the ER or urgent care center, then the patient runs the risk of having his coverage dropped or having his premiums increased because of the non-compliance issues.
Combining coverage for all aspects of health care would let the patients know that they must adhere to the treatment plans that are designed by their providers. The days of running to the doctor, only to decide not to follow the doctor's orders are over. If a patient wants to continue to have their condition covered, they must show a little responsibility for themselves.
Saturday, February 19, 2011
IRON PHARMACIST
A few days ago I had a fun exchange with another pharmacist blogger on Twitter that set the gears in motion for today's post.
Coming to APhA 2012 in New Orleans.........
IRON PHARMACIST AMERICA
Based off of the hit show Iron Chef America, IRON PHARMACIST AMERICA will pit two pharmacy teams against each other to see which team can handle the issues that face community pharmacy on any given day.
Now initially, this may seem totally boring. Who wants to watch pharmacists work? That's where we bring in the competitors. The sitting IRON PHARMACISTS will be everyday pharmacists who face the public on a daily basis. I would personally like to see pharmacists who blog as the IRON PHARMACISTS, but that's only because I would like to hear some of the commentary that may go on.
The challenger would be selected from a pool of pharmacists who seem to be the ones directing the path of pharmacy, but who don't actually see the insides of a pharmacy. Somebody from academia. Maybe one of the pharmacy organizations. Or my preferred challenger... a member of management from one of the pharmacy chains. The challenger will select which IRON PHARMACIST participates in the challenge.
Each team would have a second pharmacist, a cashier, a few techs, an intern, and a non-pharmacy manager who checks in from time to time. After a ten minute organizational meeting, each team will enter Pharmacy Stadium (located in the exposition hall so attendees can view the proceedings) and take their places inside the typical community pharmacy.
Setting for the competition is simple. Friday afternoon/evening at the pharmacy. The contest will last three hours and be recorded to be shown at a general assembly session.
During the competition, each lead pharmacist will be required to conduct one comprehensive medication review with a patient. During the competition, the pharmacy teams will conduct business as usual in a typical community pharmacy.
Of course, there may be some issues that pop-up that require the pharmacist's attention. Things like:
- Forged prescriptions for controlled substances
- Medicare B billing issues
- Family emergency requiring second pharmacist to leave early
- Medicare D eligibility issues
- Visit by the board of pharmacy, FDA, DEA, or local law enforcement
- Unannounced Medicare audit
- Non-pharmacist manager sending staff home for budgetary issues
- Discovery of a dispensing error
- Prescription that requires compounding
These issues would present themselves as the pharmacy team goes about their normal tasks of filling the prescriptions, counseling the patients, making OTC recommendations, and dealing with third-party issues.
After the competition is over, the edited video would be shown to the general assembly and a discussion would follow. It would allow for a discussion of the conditions faced by your typical community pharmacists on any given day, along with the opportunity to address these issues with the people who are "leading" the profession. If this idea is successful, a health-system edition may follow.
Because, face it folks, there is a tremendous disconnect between the pharmacists who are "leading" the profession and the pharmacists who practice the profession. It's time for the pharmacy practitioners to be heard.
There is only one question that needs to be asked.
Do you have what it takes to be the next
IRON PHARMACIST
Tuesday, February 15, 2011
Staffing
Today I'm going to share how oblivious some members of upper management are when it comes to the business of pharmacy.
At one point in my career, I was the pharmacy manager for a Wal-Mart SuperCenter. The pharmacy was open 12 hours Monday thru Friday, 10 on Saturday, and 6 on Sunday. Do the math... 76 hours per week.
We did anywhere from 1900 to 2400 scripts per week. Usually on the lower end but we would get busy from time to time.
We had three full-time pharmacists (only because we had two outstanding applicants at the same time, and this was an extremely hard to staff store... otherwise we would have had 2-1/2) and six technicians (actually five plus a summer-only intern). We were staffed well. On a typical day we had two pharmacists and 4 techs in the store.
For those of you not familiar with Wal-Mart's dispensing system, it is very labor intensive. The first step involves scanning the hard-copy prescription and entering the data into the computer. This takes one or two techs, depending on the volume at the moment. The data then goes to a pharmacist for a 4-point check where the RPh checks the tech's work.
From there the prescription gets transmitted to the third-party. If the claim is rejected, either a pharmacist or technician can resolve the issue. Once the claim adjudicates, it goes to the filling stage. We usually needed two techs to be working on this. Then back to the pharmacists to be visually verified. From there it went down to the will-call bin by the cash register, which was manned by another tech. If a patient needed counseled, we had two privacy windows for the patient to speak with the pharmacist.
At our store, to make the pharmacy run smoothly we needed to have two pharmacists and four techs in the pharmacy at any given time. During lunch breaks it was a little more hectic, but we could manage. A pharmacist would usually help out with some of the tech duties.
Well the powers-that-be from higher up the corporate ladder determined that we were overstaffed. We needed to eliminate two technician positions and split one of our pharmacists with another store. Well the one pharmacist was pregnant and had the baby so we lost her. I let the intern go and released one of the other techs, the one who usually covered the pick-up area. So now we were down to two full-time pharmacist and four technicians to cover the 76 hours that the pharmacy was open.
Wal-Mart had a couple policies that made staffing very difficult. First... no overtime. Period. Second, no hourly associate could work more than five consecutive days, even if the shifts were less than four hours.
You can imagine how much fun it was to try to schedule 4 technicians to adequately staff the pharmacy. 160 tech hours per week to cover the 76 hours that we were open, on a system that requires 4 technicians to function smoothly. We were able to grab a floater pharmacist for 10 hours per week, so we did have some overlap.
I don't know how I did it, but I was able to put together a schedule that somehow covered the pharmacy. I actually broke down the day-by-day volume and determined where we could get by with only three techs. Of course the pharmacists were doing more of the tech duties, but we were a team and it worked. I set the schedule up so that I rotated on a four week rotation. That way the techs could plan on which days and weekends they would have off. Everybody was happy.
Until one day when I went to the office to write the next week's schedule.
You see, Wal-Mart's scheduling software would schedule associates based on when the cash registers were busy. The assumption was that you needed to have more associates on hand when the customers were handing their money over to the cashiers. That works great for the general merchandise aspect of the business, but pharmacy is different.
Over my time at the store, there was never a schedule that was generated that covered the pharmacy anywhere near adequate. That's why I created my four-week rotating schedule. It covered our busy times in the pharmacy and accounted for the lulls that happen during the day and week.
On this day, I walked back to the office to enter the schedule into the computer. As I sat down, the DM for the entire store walked into the office. He saw that I had my hand-written schedule and was starting to enter it into the computer.
He came back and asked me what I was doing. Of course I told him that I was putting in the pharmacy schedule. He questioned me why I wasn't using the computer generated schedule. After all, the computer knows everything.
Except the business of pharmacy. The only factor that the computer used in determining pharmacy staffing was when the prescriptions were actually rang out of a register. We all know that mornings are hectic in the pharmacy, mostly from the overnight refills. Then the evening rush happens as everybody comes in to pick up their medications that either they or their physician called in.
For this particular schedule, the computer said to staff the pharmacy with 5 technicians (remember I only have 4 now) from 6:30 PM until 8:30 PM on Monday. We closed at 8:00. It also said that I only needed one technician on Monday from 11:30 AM until noon. Zero techs for the rest of Monday, at least until 4:00 PM. Aren't Monday mornings usually a little busy? But since the actual sale didn't occur until the prescription was rung thru a register, the computer didn't know how to schedule.
The store's manager and two assistant managers were with the DM. They knew that I had turned in my resignation the previous Monday and that this was the last schedule that I would write. But we sat there and let the DM go on for 45 minutes about how awesome the scheduling program was. When he finished, I told him that the next day was my last day with Wal-Mart.
When I returned to the pharmacy department, everybody questioned me why it took so long to put in the schedule this week. I told them what the DM had done.
We had a good laugh. This DM could be the worst one that I ever had.
Tuesday, February 8, 2011
MTM opportunity?
Others may think of disease state management programs when they think about MTM. Programs where the pharmacist works with the patient to treat a specific disease...diabetes, asthma/COPD, hypertension, or hyperlipidemia.
Most of the talk that I see about medication therapy management revolves around the community pharmacy setting. But what about in the hospitals?
I write this with a specific case in mind. A case where pharmacist involvement could have saved the patient, the community pharmacist, and several nurses a significant amount of time on a weekend.
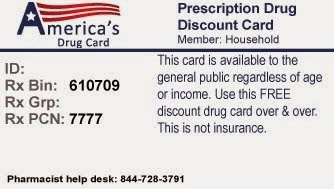
First the details of the case. Patient is admitted and has several stents placed. Patient does not tolerate clopidogrel, so the patient is started on prasugrel. The patient is insured by a government-funded program that does not cover prasugrel without a prior authorization. After spending a few days as an inpatient, the patient is discharged on Saturday afternoon.
For those who work in a community pharmacy, you know what happens next. The pharmacy processes the claim for the prasugrel and receives the "Prior Authorization required" message. Now the community pharmacist gets to tell the patient's spouse that the medication is not covered, knowing that it will take several days for the prior authorization to be approved. The labeling of the prasugrel states that it must be stored in the original container with the desiccant. We inform the patient's spouse that they can pay the retail price now, then get a refund once the claim is approved.
That didn't go over well. About ninety minutes later the pharmacy receives a call from a nurse case manager who is fairly hot over the issue. The patient neeeeds this medication. I don't doubt that one bit, but it requires a prior authorization. So the nurse case manager says that she will take care of the PA.
Another hour passes and the nurse case manager calls back. The PA desk is closed for the weekend. That doesn't surprise me one bit. The nurse case manager calls back. What are we going to do? The patient neeeeds this medication. The patient just had several stents placed.
This is where I want to throw the lack of preparation on your part doesn't constitute an emergency on my part back in the nurse case manager's face. But I have a patient who needs their medication. I don't want a couple hundred bucks of medication go out the door without having some sort of arrangement set up, just in case the prior authorization isn't approved. In the end, the patient went home with the prasugrel after the financials had been worked out.
Where was the pharmacist in this case? Did the hospital pharmacist have any role in the discharge planning for this patient? If they did, did they do anything other than glance at the chart a few times during the time that the patient was admitted.
I've said this before and I'll say it again. A medication regimen that the patient can afford and will take regularly is far more effective than the clinically superior regimen that the patient can't afford and won't take. That's one of the keys to my view of medication therapy management.
As soon as it was determined that the prasugrel would be the patient's home-going medication, somebody at the hospital (pharmacist) should have checked to see if the medication would be covered by the patient's insurer. It took me under 15 seconds to see that the medication would be covered with a prior authorization, and I was able to see what the copay would be once approved.
That's part of the practice of medication therapy management. Making sure the patient can afford the medications. It's a place where the hospital pharmacists can impact the care that the patients receive, but it may be beneath the duties of a clinical pharmacist.
I practice community pharmacy in a very rural area. The closest major teaching hospital is over sixty miles away. There are five cities with major teaching facilities within two hours of my pharmacy. These cities have eight hospitals that I would say are top-notch. Of these eight hospitals, only two of them regularly have prior authorizations taken care of prior to the patient being discharged.
Hello hospital pharmacy directors. If only two of the eight major teaching facilities take care of PAs prior to discharge, you can imagine how well the local city/county hospitals take care of PAs.
MTM pharmacists....maybe this is an area where you can expand your practice.
Tuesday, February 1, 2011
A calming environment
He remained outside for the past seven years, but a couple weeks ago we decided to bring him back inside. Actually, our daughter cried and cried until we caved in. A trip to the groomer to get a haircut and the dog is back inside.
When he was younger, he was rambunctious. Now he just lays around. When I'm sitting in my chair, he will come over and put his head on my lap. After petting him for a little bit, he will lay down again. The kids will go over and use him as a pillow and watch the television.
He likes it. He's getting the attention that he has missed over the last several years. Since he has come back into the house, he has been a calming influence. The boys aren't arguing as much. I find that I'm not yelling at the kids as much either. It's like the dog is our family tranquilizer.
Makes me wonder if having animals around the pharmacy department would have the same type of calming effect.
Maybe not dogs.
Maybe some fish.
A couple larger fish tanks. Some color schemes that bring tranquility to the pharmacy instead of the bright white paint with fluorescent lights that gives the pharmacy a bleak appearance. I see blues and greens around the fish.
Perhaps a Tuscan color scheme could be brought to the pharmacy. Canned lighting. Maybe artwork on the walls that has some accent lighting.
Anybody works in a place like this? What's it like?