Recently, both the Journal of the American Pharmacists Association and the American Journal of Health-Systems Pharmacy have had articles that have discussed the use of blogs by pharmacists. After reading the articles and their conclusions, I decided to share my thoughts on the topic.
First for some personal blogging history. Up until four years ago, I didn't even know what a blog was. Then I had to take some time off for knee surgery and was out of the pharmacy for three months. My physician did not allow me to drive my vehicle for the first 2-1/2 months, so I spent a lot of time, I mean a lot of time in my house playing on the computer.
One day I was searching for something and I stumbled upon a blog written by a nurse in Pennsylvania. It was written very well and gave some insights into her profession. I followed some of the links on her page and read other nurse and physician blogs. Eventually I found a couple pharmacy blogs that I liked and began to read them. Once I returned to work, it didn't take me long to start my own blog.
With my first blog, I remained anonymous. Just like all of the other blog authors. I used the blogging process to vent my frustrations with my job. Bad experience with a patient... I'd change details but still vent about it. Insurer screwing the pharmacy over... blog post. All of the little things that got under my skin were fair game. Some days I would post minutes after an incident happened in the pharmacy.
Then I had an article that I submitted to Drug Topics get published. The email response to my article was amazing. That article was the first time that I had my own thoughts attributed to my own name. I liked the idea that people would know who was behind the thoughts. It didn't take long for me to stop writing that blog, remove most of the posts, and no longer identify with that blog persona.
But enough of my history. Let's get back to the two articles.
Both articles mention the negativity of the content of the blogs. I totally understand where the blog authors are coming from. A lot of pharmacists feel like their comments are not taken seriously by upper levels of management. The blog posts are a means to share feelings and frustrations without revealing who you are. If you send an email in a corporate setting, your name is attached to your comments forever. The anonymity of blogging is a security blanket. The comments that follow a post let the author know that they are not alone in their thoughts.
In blog posts, pharmacists share their interactions with patients. Most of the time these posts may appear to paint the patient in a not-so-good manner. I hate to say it, but my experiences over the past 15+ years as a licensed pharmacist mimic those that are blogged. Patient health literacy is poor. People aren't concerned about their disease states, they just want a pill to fix their problems. People don't want to accept personal responsibility for their health conditions. And as long as the manufacturers are able to continue with their DTC advertising, why should people take the responsibility? These types of posts are simply a commentary on what our society has become.
The articles mention that the pharmacy blogs are an early warning system for what is happening in the profession of pharmacy. I totally agree. I honestly believe that the pharmacist bloggers can spread the word on workplace and professional issues much better than any organization. When a pharmacist blogs, there is no peer-review process that slows down the publication. If I have a thought to share, it's out there as fast as my fingers can fly over my keyboard. Journals and other publications take months to share information.
With the speed that the health-care system is changing, we can't sit back and wait for the national and state pharmacist organizations to evaluate, study, form an opinion on new legislation, then share it with the pharmacists. Pharmacists need a fluid environment to get thoughts out to be discussed. Blogs provide that.
As for professionalism within the blog posts. I can only speak for myself and say that I try to remain professional. I keep the language clean and try not be overly critical of patients. I'm putting my name to my writing and I am owning my words. When you identify who you are, you watch what you say. Some other bloggers use more colorful language in their posts. I don't pay much attention to the words as to the message that the author is trying to convey.
As I mentioned in my state of the profession series, local pharmacist organizations are practically non-existent these days. The chains have scheduled pharmacists to the point that we don't have time to meet after work to discuss issues that we face as a profession. Maybe that's the role that pharmacist blogs are playing in our digital world. The combination of different types of blogs is simply a reflection of the different personalities that would be at the meeting. Some people are story-tellers. Some people share currents trends in the workplace. Others just sit back and take it all in. By evaluating all of the commentary that is put out there, blog readers can get a pretty good idea of what is happening in the profession.
Tuesday, December 28, 2010
Saturday, December 25, 2010
Today, take a minute
Take a minute and say a little prayer for the members of the United States military who are deployed all over the world. You don't have to agree with the politics that have sent them where they are, but they joined voluntarily to serve our country. For that they deserve our gratitude and prayers not only today, but every day.





Remember those who have fallen

And the families they leave behind









Remember those who have fallen

And the families they leave behind




Friday, December 24, 2010
Christmas story
Here's a few pictures that I stole from The Chive to look at while listening to one of my favorite renditions of the story of Christmas.















Merry Christmas.















Merry Christmas.
Wednesday, December 22, 2010
End of the year insurance tips
It started yesterday at my pharmacy. Medicare Part D patients started bringing in their new cards and wanting us to bill their new prescription plan for their prescriptions. Of course, all of the claims came back to us saying that the coverage was not in effect yet. And then the pharmacy staff had to spend a minimum of five minutes explaining to the patient why the claims would not go through. Then another five minutes telling the spouse/son/daughter the same thing.
So in an effort to save all of us some headaches as this benefit year winds down and a new one gets ready to ramp up, I've decided to share a few tips for the pharmacy patients out there to make the year-to-year transition go a little bit easier.
Tip #1
If you a currently in the donut hole and have enough medication to carry you into the new year, please wait until the new year to get your refills. You will save yourself money. Any expenses in December do not count towards your deductible in January.
Every year it happens. Sometime between Christmas and New Year's Eve I have a patient call in for a refill on their Plavix. Of course it's written for a three month supply. The patient will pick-up the medication and pay the $400+ copay. Then on the first Sunday of the new year, their adult child will call in to complain that we charged their mother or father such a high copay, and that we should have known and just filled enough to cover them until their new coverage/benefit year goes into effect.
Ummm....no. You need to be responsible for yourself/your parent. It's not my job to watch out for that. Personally, I don't even look to see what the copays are when I'm checking the prescriptions. It's my job to make sure the right medication is going to the right person at an age-appropriate dose. It's my job to make sure that there are no drug interactions or contraindications for therapy on the prescriptions. It's my job to educate and inform the patient about their medication if they accept the offer of counseling. It's not my job to pay attention to your/your parent's finances. When the cashier tells you what the price is for your medications, that's when you should say something. Waiting for a week, then calling in to complain about the price isn't going to change anything.
Tip #2
This one goes hand-in-hand with the first one. If you call ahead for a refill and don't plan on picking it up until after the start of the new year, it's still going to be billed to the previous year's coverage. In pharmacy, we bill your insurance on the day that we fill the prescription. We don't wait until you come in to pick it up, then file a claim. Every year my pharmacy wastes hours and hours of labor unfilling prescriptions that were billed to the previous benefit year and refilling them under the current benefit year.
Tip #3
Don't come in to the pharmacy during the first week of the new year unless it is absolutely necessary.
I've been at this for a long time and there is one thing that you can bank on every single year. The insurance companies do not have all of the eligibility information loaded into their computers at the start of the year.
I agree with you, they should have the information updated.
But they don't.
It creates the proverbial clusterduck.
It's not the pharmacy staff's fault, so don't gripe at us about it. Call your insurer and make sure that your eligibility has been updated. Or stand there and stare at the pharmacy staff as we make the phone call that you could just as easily make. Just don't gripe while we are trying to help you and a dozen other people who have the same issue.
And if you decided to wait until the last day of the Medicare Part D enrollment period (December 31) to sign up, don't expect your coverage to be updated at 10 AM on New Year's Day.
Tip #4
If you have your 30 day supply of Vicodin filled on December 20th and want us to refill it on January 3 using your new insurance, it's not going to happen. We're going to make you wait until the refill is due. Don't waste my time. I'm the Vicodin/Xanax/Tramadol/Percocet cop.
Tip #5
If you managed to stay out of the donut hole for the previous benefit year and have your prescriptions refilled in the middle of December, don't try to squeeze in one more refill before the end of the year, before your copays go up.
The insurance companies know that you will try this. They aren't going to pay for an early refill. Ever.
Hopefully these tips will help ease the transition into a new benefit year for you.
So in an effort to save all of us some headaches as this benefit year winds down and a new one gets ready to ramp up, I've decided to share a few tips for the pharmacy patients out there to make the year-to-year transition go a little bit easier.
Tip #1
If you a currently in the donut hole and have enough medication to carry you into the new year, please wait until the new year to get your refills. You will save yourself money. Any expenses in December do not count towards your deductible in January.
Every year it happens. Sometime between Christmas and New Year's Eve I have a patient call in for a refill on their Plavix. Of course it's written for a three month supply. The patient will pick-up the medication and pay the $400+ copay. Then on the first Sunday of the new year, their adult child will call in to complain that we charged their mother or father such a high copay, and that we should have known and just filled enough to cover them until their new coverage/benefit year goes into effect.
Ummm....no. You need to be responsible for yourself/your parent. It's not my job to watch out for that. Personally, I don't even look to see what the copays are when I'm checking the prescriptions. It's my job to make sure the right medication is going to the right person at an age-appropriate dose. It's my job to make sure that there are no drug interactions or contraindications for therapy on the prescriptions. It's my job to educate and inform the patient about their medication if they accept the offer of counseling. It's not my job to pay attention to your/your parent's finances. When the cashier tells you what the price is for your medications, that's when you should say something. Waiting for a week, then calling in to complain about the price isn't going to change anything.
Tip #2
This one goes hand-in-hand with the first one. If you call ahead for a refill and don't plan on picking it up until after the start of the new year, it's still going to be billed to the previous year's coverage. In pharmacy, we bill your insurance on the day that we fill the prescription. We don't wait until you come in to pick it up, then file a claim. Every year my pharmacy wastes hours and hours of labor unfilling prescriptions that were billed to the previous benefit year and refilling them under the current benefit year.
Tip #3
Don't come in to the pharmacy during the first week of the new year unless it is absolutely necessary.
I've been at this for a long time and there is one thing that you can bank on every single year. The insurance companies do not have all of the eligibility information loaded into their computers at the start of the year.
I agree with you, they should have the information updated.
But they don't.
It creates the proverbial clusterduck.
It's not the pharmacy staff's fault, so don't gripe at us about it. Call your insurer and make sure that your eligibility has been updated. Or stand there and stare at the pharmacy staff as we make the phone call that you could just as easily make. Just don't gripe while we are trying to help you and a dozen other people who have the same issue.
And if you decided to wait until the last day of the Medicare Part D enrollment period (December 31) to sign up, don't expect your coverage to be updated at 10 AM on New Year's Day.
Tip #4
If you have your 30 day supply of Vicodin filled on December 20th and want us to refill it on January 3 using your new insurance, it's not going to happen. We're going to make you wait until the refill is due. Don't waste my time. I'm the Vicodin/Xanax/Tramadol/Percocet cop.
Tip #5
If you managed to stay out of the donut hole for the previous benefit year and have your prescriptions refilled in the middle of December, don't try to squeeze in one more refill before the end of the year, before your copays go up.
The insurance companies know that you will try this. They aren't going to pay for an early refill. Ever.
Hopefully these tips will help ease the transition into a new benefit year for you.
Saturday, December 18, 2010
Bad Pharmacist
It looked a little odd. It was written on the prescription blank as a transfer in to our pharmacy, but it only said from CVS in a town on the other side of the state. No prescription number. No pharmacy phone number. Prescription was for Stadol NS. Plus, it was for the other pharmacist's husband. Hmmmm.
I photocopied the prescription and placed it into a file. I might need to keep this for later, I thought.
Two weeks later I was reviewing the previous weekend's prescriptions (we were a slow pharmacy so we were able to do all of the QA stuff that corporate wanted). There was one of our refill authorization forms with an "OK x 1 by MD" written on the face of the form. I did a little checking. The prescription was processed at 2:15 on Saturday afternoon. So I called the doctor's office. They had released both my partner and her husband as patients over 12 months prior. I spoke directly with the physician and he stated that he did not authorize the medication over the weekend.
From there it took one phone call to the pharmacy board and 5 days later, my partner had her license suspended. The BoP had been investigating this pharmacist when she worked on the other side of the state, but she moved before they could make a case against her. Since our inspector's have such a gigantic caseload, her file did not get forwarded to our local BoP agent.
And my employer did not do a background check on this pharmacist. They hired her simply because she was breathing and had a license. I had known her back in college, but she fell behind after our first or second year so I lost track of her. Never would have suspected her of stealing medications or forging prescriptions.
She has since completed a rehab program and had her license reinstated.
The best part..... when the BoP agent came to the pharmacy to bust her, our DM was requested to be present. And he was hauling around one of the corporate VPs that day. She had to sit in the store's dingy office for two hours while the bust went down. HA!
I photocopied the prescription and placed it into a file. I might need to keep this for later, I thought.
Two weeks later I was reviewing the previous weekend's prescriptions (we were a slow pharmacy so we were able to do all of the QA stuff that corporate wanted). There was one of our refill authorization forms with an "OK x 1 by MD" written on the face of the form. I did a little checking. The prescription was processed at 2:15 on Saturday afternoon. So I called the doctor's office. They had released both my partner and her husband as patients over 12 months prior. I spoke directly with the physician and he stated that he did not authorize the medication over the weekend.
From there it took one phone call to the pharmacy board and 5 days later, my partner had her license suspended. The BoP had been investigating this pharmacist when she worked on the other side of the state, but she moved before they could make a case against her. Since our inspector's have such a gigantic caseload, her file did not get forwarded to our local BoP agent.
And my employer did not do a background check on this pharmacist. They hired her simply because she was breathing and had a license. I had known her back in college, but she fell behind after our first or second year so I lost track of her. Never would have suspected her of stealing medications or forging prescriptions.
She has since completed a rehab program and had her license reinstated.
The best part..... when the BoP agent came to the pharmacy to bust her, our DM was requested to be present. And he was hauling around one of the corporate VPs that day. She had to sit in the store's dingy office for two hours while the bust went down. HA!
Wednesday, December 15, 2010
Reimbursement for OTC consults
One my last post, I proposed a means by which individual pharmacists can be reimbursed personally for the professional services that they provide on each and every prescription. By including our personal NPIs on claims, insurance companies would reimburse us for DUR review, interventions, etc...
But that only encompasses part of the professional aspects of our profession. Those are duties required to accurately process a prescription medication order. As pharmacists, we currently give away our professional knowledge without being compensated for it. I have a possible means by which we can be reimbursed for what we are currently giving away.
I'm talking about our OTC consults.
Think about a typical consult. We gather pertinent information about both the condition and the patient that we are being asked to help treat. Think of it as taking a history of the patient and condition. After gathering this information, we basically diagnose what we are being asked to treat. Most of the time we can select an OTC product, but other times we refer the patient (notice...patient, not customer) to be evaluated because the condition is more complex and beyond the scope of our practice.
And we do this for free.
Why?
If this patient went to the ER, urgent care, or their physician, the same triage process would be done. Most of it by a nurse. The prescriber would come in, take a look at the patient, make a diagnosis and move on. For this the physician would bill anywhere from $70 to $180, depending on the complexity of the visit. More if it was done in an ER.
Why can't we bill for our triage. Think of the hundreds and thousands of dollars we save the health care system every day by keeping people away from the ERs. We are individual health care providers, but we just haven't decided to bill for our services.
It's time.
But that only encompasses part of the professional aspects of our profession. Those are duties required to accurately process a prescription medication order. As pharmacists, we currently give away our professional knowledge without being compensated for it. I have a possible means by which we can be reimbursed for what we are currently giving away.
I'm talking about our OTC consults.
Think about a typical consult. We gather pertinent information about both the condition and the patient that we are being asked to help treat. Think of it as taking a history of the patient and condition. After gathering this information, we basically diagnose what we are being asked to treat. Most of the time we can select an OTC product, but other times we refer the patient (notice...patient, not customer) to be evaluated because the condition is more complex and beyond the scope of our practice.
And we do this for free.
Why?
If this patient went to the ER, urgent care, or their physician, the same triage process would be done. Most of it by a nurse. The prescriber would come in, take a look at the patient, make a diagnosis and move on. For this the physician would bill anywhere from $70 to $180, depending on the complexity of the visit. More if it was done in an ER.
Why can't we bill for our triage. Think of the hundreds and thousands of dollars we save the health care system every day by keeping people away from the ERs. We are individual health care providers, but we just haven't decided to bill for our services.
It's time.
* * * * *
In case you've missed it, this past March a little bill was passed and signed into law that basically provides health care to all Americans. Like it or not, it's now the law. Even with the Virginia ruling on the constitutionality of one of the provisions, the law is still in effect. One of the provisions of the bill is the implementation of electronic health records.
How these are going to work, I haven't a clue. But pharmacy/pharmacists have the opportunity to capitalize on this. This may seem a little bit Big Brotheresque, but it is what it is. If we are going to be required to maintain electronic health records, let's go all in with it.
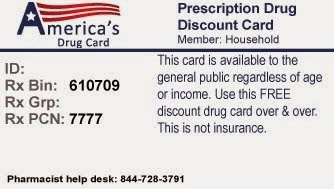
I propose that all persons should have a card, similar to a credit card, that has their insurance information embedded on it. The information can only be modified by certain entities, such as insurance carriers and benefits administrators. If a person has coverage, it is recorded on the card. If coverage has been dropped, the administrator modifies the data. Get a new job, you take your card to your new benefits administrator to have the information added to your card.
The card is required for all transactions surrounding a person's health care. That way a person can't jump from provider to provider, using insurance at one place and claiming to be self-pay at another. The card would simply carry the patient's insurance information and record which providers they have seen. No medical information would be captured on the card. But in the event of an emergency, it would provide information about where the patient had been seen. Phone calls could then be made. No more calls to see if Mr Jones had his prescriptions filled at CVS, Walgreens, or Target. The ER would know simply by swiping the card.
Your thoughts?
How these are going to work, I haven't a clue. But pharmacy/pharmacists have the opportunity to capitalize on this. This may seem a little bit Big Brotheresque, but it is what it is. If we are going to be required to maintain electronic health records, let's go all in with it.
I propose that all persons should have a card, similar to a credit card, that has their insurance information embedded on it. The information can only be modified by certain entities, such as insurance carriers and benefits administrators. If a person has coverage, it is recorded on the card. If coverage has been dropped, the administrator modifies the data. Get a new job, you take your card to your new benefits administrator to have the information added to your card.
The card is required for all transactions surrounding a person's health care. That way a person can't jump from provider to provider, using insurance at one place and claiming to be self-pay at another. The card would simply carry the patient's insurance information and record which providers they have seen. No medical information would be captured on the card. But in the event of an emergency, it would provide information about where the patient had been seen. Phone calls could then be made. No more calls to see if Mr Jones had his prescriptions filled at CVS, Walgreens, or Target. The ER would know simply by swiping the card.
* * * * *
This idea may seem a little far-fetched, but we (as pharmacists) need to start looking out for the economic survival of our profession. The AMA just had the cuts in physician reimbursement delayed because they pay attention to the money. We need to do the same.So how does this apply to pharmacy and pharmacist reimbursement?
Glad you asked. Whenever we provide any professional services for anything other than that which is mandated by OBRA, we must be presented with the card. No card = no service.
Basically we swipe the card on a PDA-type device to gather the patient's information. Conduct our OTC consult as normal, but at the end we record the details of our consultation. Depending on the length of time and complexity of the consult, we bill the insurance appropriately for our services. The details we provide determines the reimbursements that we receive. At the end of the day, we upload our interactions for the day and submit the claims. All claims are tied to our individual NPIs, so reimbursements are sent directly to individual pharmacists.
(For people without insurance, the data is still recorded for the sake of electronic health records. Rather than bill for the intervention, pharmacists receive a tax break as "charity care")
This post only addresses the community pharmacy aspect, but it can be easily adapted to clinical and consultant services.
Glad you asked. Whenever we provide any professional services for anything other than that which is mandated by OBRA, we must be presented with the card. No card = no service.
Basically we swipe the card on a PDA-type device to gather the patient's information. Conduct our OTC consult as normal, but at the end we record the details of our consultation. Depending on the length of time and complexity of the consult, we bill the insurance appropriately for our services. The details we provide determines the reimbursements that we receive. At the end of the day, we upload our interactions for the day and submit the claims. All claims are tied to our individual NPIs, so reimbursements are sent directly to individual pharmacists.
(For people without insurance, the data is still recorded for the sake of electronic health records. Rather than bill for the intervention, pharmacists receive a tax break as "charity care")
This post only addresses the community pharmacy aspect, but it can be easily adapted to clinical and consultant services.
* * * * *
Your thoughts?
Thursday, December 9, 2010
Pharmacist reimbursement for professional aspects of dispensing
By now I think that anybody who reads this blog knows that I believe that pharmacists should be getting reimbursed for all of the professional activities that we engage in. In the community practice setting, a dispensing fee just doesn't cut it any longer, especially when the drugs are being reimbursed thru WAC, MAC, and GEAP-minus formulas.
The effect of the $4 generic programs has reduced the profession to a product. People aren't valuing the professional expertise of the pharmacists, they are frequenting the pharmacies that sell the product cheaply. In my state, a regional chain has started offering $2 generic prescriptions. Couple that with the free diabetes medications at a certain Pittsburgh-based chain and free generic antibiotics offered by several pharmacies and I can see why the public doesn't value our services.
It's because we don't value our services.
I honestly don't see pharmacy rebounding to the point where a respectable dispensing fee will ever be offered to pharmacies. The chains and insurers have seen to it that we will accept horrible reimbursements, so why should we expect to ever see a decent dispensing fee again?
What I propose is to remove pharmacist services from the equation when it comes to setting reimbursements to the pharmacy for the product. CVS, Walgreens, Target, Walmart, whoever can accept whatever reimbursements they want for the product, because we (the pharmacists) would be getting reimbursed for the professional functions on each and every prescription.
The NPI number of the pharmacist is included on every claim that is submitted to the insurer. This is in addition to the pharmacy's NPI that is submitted for product reimbursement. Prior to submitting a claim, all of the pharmacist's professional functions are summarized and coded to be submitted with the claim (software determines the coding). Based on the level of pharmacist intervention, the pharmacist will be reimbursed personally for his/her intervention.
If the pharmacist doesn't want to be reimbursed for their professional services, they can opt to submit the facility's NPI instead of their own. But once pharmacists see other pharmacists raking in the money from their interventions, all pharmacists would be submitting their own NPIs on the claims.
For example, a mother drops off a prescription for cefdinir 250mg/5ml 2.6 ml qd x 10 days. The prescription is entered for a quantity of 60 ml (the smallest package available) for the 10 day supply.
The pharmacy dispensing system flags the order as being an overdose for the patient age. Pharmacist reviews the dose and documents that the dose is appropriate for the patient's age and weight and that the days supply is 10 days due to both the prescription order and the expiration dating of the reconstituted product.
When the claim is submitted, the pharmacy is reimbursed to the product at the contract price. The pharmacist receives payment for verifying the dose and day supply. There would have to be a means to edit the intervention info based on the OBRA-mandated counseling session (maybe professional service claims get submitted every Saturday night), but I think you get the drift of where I would like to see this going.
Anybody know if an idea like this has ever been explored?
The effect of the $4 generic programs has reduced the profession to a product. People aren't valuing the professional expertise of the pharmacists, they are frequenting the pharmacies that sell the product cheaply. In my state, a regional chain has started offering $2 generic prescriptions. Couple that with the free diabetes medications at a certain Pittsburgh-based chain and free generic antibiotics offered by several pharmacies and I can see why the public doesn't value our services.
It's because we don't value our services.
I honestly don't see pharmacy rebounding to the point where a respectable dispensing fee will ever be offered to pharmacies. The chains and insurers have seen to it that we will accept horrible reimbursements, so why should we expect to ever see a decent dispensing fee again?
What I propose is to remove pharmacist services from the equation when it comes to setting reimbursements to the pharmacy for the product. CVS, Walgreens, Target, Walmart, whoever can accept whatever reimbursements they want for the product, because we (the pharmacists) would be getting reimbursed for the professional functions on each and every prescription.
The NPI number of the pharmacist is included on every claim that is submitted to the insurer. This is in addition to the pharmacy's NPI that is submitted for product reimbursement. Prior to submitting a claim, all of the pharmacist's professional functions are summarized and coded to be submitted with the claim (software determines the coding). Based on the level of pharmacist intervention, the pharmacist will be reimbursed personally for his/her intervention.
If the pharmacist doesn't want to be reimbursed for their professional services, they can opt to submit the facility's NPI instead of their own. But once pharmacists see other pharmacists raking in the money from their interventions, all pharmacists would be submitting their own NPIs on the claims.
For example, a mother drops off a prescription for cefdinir 250mg/5ml 2.6 ml qd x 10 days. The prescription is entered for a quantity of 60 ml (the smallest package available) for the 10 day supply.
The pharmacy dispensing system flags the order as being an overdose for the patient age. Pharmacist reviews the dose and documents that the dose is appropriate for the patient's age and weight and that the days supply is 10 days due to both the prescription order and the expiration dating of the reconstituted product.
When the claim is submitted, the pharmacy is reimbursed to the product at the contract price. The pharmacist receives payment for verifying the dose and day supply. There would have to be a means to edit the intervention info based on the OBRA-mandated counseling session (maybe professional service claims get submitted every Saturday night), but I think you get the drift of where I would like to see this going.
Anybody know if an idea like this has ever been explored?
Friday, December 3, 2010
Take a moment to smile
One of the issues I face writing this blog is finding the time to sit down and actually post. And when I do have the time to sit down, I sometimes get writer's block.
Now is one of those times.
I have ideas for pharmacist billing of services sketched out on a legal pad, but translating it into a post isn't happening right now.
So today I'm going to share a comic that used to be taped on the wall, next to my desk back when I was a student at Ohio Northern University. Hopefully you will like it.

Now is one of those times.
I have ideas for pharmacist billing of services sketched out on a legal pad, but translating it into a post isn't happening right now.
So today I'm going to share a comic that used to be taped on the wall, next to my desk back when I was a student at Ohio Northern University. Hopefully you will like it.

Subscribe to:
Posts (Atom)