So what is happening? A branch of the Mayo Clinic will stop accepting payments from Medicare after the turn of the year. Here's the link.
But why would anybody opt out of a contract with the government?
Ummm.. the article tells you exactly why
- Low payments
- Slow payments
Personally, I'm happy to see a provider step away from a contract that loses money. It's not a good business model to operate at a loss. I took one economics/business class during my second year of college and if I learned anything it was that you can't continue to run a business if continually loses money.
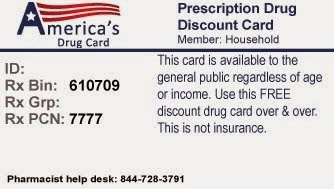
If only somebody in the pharmacy world would take a look at insurance contracts before just blindly signing on the dotted line. At my previous position, our wholesaler offered a service where they took care of all of our third-party contracts. Nobody at my company even looked at the terms before we were locked into another year of the take-it-or-leave-it terms dictated by the insurance company. And then they wonder why reimbursements are falling.
Pharmacists need to speak up when they see the piss-poor reimbursements from the insurers. Between the $4 generics and the free antibiotics, we're digging ourselves into a hole.
When an insurer sees that one provider is willing to provide a product or service for a low fee, the insurer starts steering the contract language to drive our reimbursements down to that level.
We, as pharmacists, think that we are being competitive by driving our prices down. We think that lower prices will attract more patients, which in turn will increase revenue. We are playing into the hands of the insurance companies. They have teams of accountants, actuaries, and lawyers whose jobs are to decrease the insurers expenditures. Who's looking out for us? Sally at Drug Wholesale Company?
The point of this post is this... we can have a pie-in-the-sky view that people want to pay us based on our clinical knowledge, and that can be our end goal. But right now, our services are tied to a product. And we need to make sure that the reimbursement for the product includes an adequate fee for our clinical skills that we use on each and every prescription that crosses in front of us. If the contract isn't good enough, we don't need to sign it.
Mayo Clinic, I applaud you for having the boys to pass on an poor contract. Hopefully more providers follow your lead.